Pericarditis:-
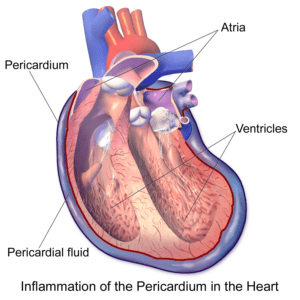
Pericarditis means the heart’s outer sac, called the pericardium, gets swollen and irritated, causing sharp chest pain when its layers rub together.
Table of Contents
ToggleUsually, pericarditis isn’t severe and can go away on its own without treatment. But in more serious cases, treatment might involve medicines or, in rare situations, surgery. It’s important to detect and treat pericarditis early to lower the chances of future complications.
Pericarditis Symptoms:-
The main sign of pericarditis is chest pain, which can feel sharp or stabbing, but for some, it might be dull, achy, or like pressure in the chest.
This pain usually sits behind the breastbone or on the left side of the chest and may:
- Travel to the left shoulder and neck
- Worsen with coughing, lying down, or deep breaths
- Improve when sitting up or leaning forward
Other symptoms of pericarditis can include:
- Coughing
- Feeling tired or weak
- Swelling in the legs
- Slight fever
- Heart palpitations (rapid or irregular heartbeat)
- Trouble breathing while lying down
- Swelling in the belly
The symptoms of pericarditis differ depending on its type, categorized by symptom patterns and duration.
Acute pericarditis starts suddenly but typically lasts no more than three weeks. It might recur, making it challenging to differentiate from a heart attack.
Recurrent pericarditis shows up around four to six weeks after an acute episode, with no symptoms in between.
Incessant pericarditis lasts for about four to six weeks but persists continuously without breaks.
Chronic constrictive pericarditis develops gradually and lasts longer than three months.
Types of pericarditis:-
- Acute pericarditis: A sudden inflammation of the pericardium accompanied by immediate symptoms.
- Chronic pericarditis: Inflammation of the pericardium persists for three months or more after the initial acute phase.
- Constrictive pericarditis: A severe form of pericarditis where inflamed pericardial layers stiffen, develop scar tissue, thicken, and adhere together, disrupting normal heart function. Often occurs after repeated acute pericarditis episodes.
- Infectious pericarditis: Develops due to viral, bacterial, fungal, or parasitic infections.
- Idiopathic pericarditis: Pericarditis without a known cause.
- Traumatic pericarditis: Arises following chest injuries, like those from car accidents.
- Uremic pericarditis: Occurs due to kidney failure.
- Malignant pericarditis: Results from cancer growth within the body

How to sleep with pericarditis:-
Dealing with pericarditis can impact sleep. Here are some suggestions on how to sleep with pericarditis:
- Position: Lie on your side with a pillow for support or try propping yourself up slightly with pillows to ease discomfort.
- Relaxation Techniques: Practice relaxation methods like deep breathing or gentle stretching before bedtime to calm the body.
- Medications: Take prescribed pain relievers or anti-inflammatories as recommended by your doctor to manage discomfort and aid sleep.
- Comfortable Environment: Ensure a quiet, dark, and comfortable sleeping environment to promote restfulness.
- Sleep Aids: Consider using sleep aids or techniques like white noise or soothing music to help drift off.
- Consult a Specialist: Discuss specific sleeping positions or techniques with your healthcare provider for personalized advice.
Pericarditis ecg:-
An electrocardiogram (ECG) plays a crucial role in diagnosing pericarditis, a condition where the pericardium, the sac around the heart, becomes inflamed.
On an ECG, specific changes often indicate pericarditis. These changes may include:
- Elevated ST Segments: These can appear widespread or be more noticeable in certain leads.
- Depressed PR Segment: This may be seen in some leads.
- Diffuse T-Wave Inversions: Inverted T-waves might appear across multiple leads.
However, an ECG alone might not confirm pericarditis. Additional tests and a medical evaluation are usually needed for a comprehensive diagnosis.

What is myocarditis and pericarditis?:-
Myocarditis and pericarditis both involve inflammation in the heart, but they affect different parts. Myocarditis occurs in the heart muscle, while pericarditis affects the lining around the heart, known as the pericardium. Viruses commonly cause both conditions. While they both result in chest pain, pericarditis-related pain often eases when sitting up and leaning forward. Myocarditis, on the other hand, tends to make you feel tired and weak.
What cause pericarditis:-
- Viral pericarditis often develops as a complication of viral infections, commonly gastrointestinal viruses.
- Bacterial pericarditis results from bacterial infections like tuberculosis.
- Fungal and parasitic infections can also lead to specific types of pericarditis.
- Autoimmune diseases like lupus, rheumatoid arthritis, and scleroderma might cause pericarditis.
- Traumatic pericarditis arises from chest injuries, such as those in car accidents.
- Uremic pericarditis links to kidney failure.
- Malignant pericarditis can stem from tumors like lymphoma.
- Genetic conditions such as Familial Mediterranean Fever (FMF) may trigger pericarditis.
- Rarely, medications suppressing the immune system can induce pericarditis.
Moreover, the risk of pericarditis increases after certain events:
- Following a heart attack.
- Postpericardiotomy syndrome after open heart surgery.
- After radiation therapy or specific procedures like cardiac catheterization or radiofrequency ablation (RFA).
In these cases, pericardial inflammation may be the body’s response to the procedure or condition. Symptoms of pericarditis can sometimes manifest weeks after bypass surgery. If concerned, discussing this with a surgeon is recommended.
Pericarditis diagnosis:-
Detecting pericarditis involves recognizing specific symptoms that differ from a heart attack. These include sharp chest pain extending to the shoulders, easing when sitting up or leaning forward, and chest discomfort intensifying with breathing.
During an assessment, your Doctor considers your symptoms, recent illnesses, and your medical history, including heart conditions, surgeries, and other health issues that might increase pericarditis risk.
The doctor will listen to your heart, aiming to detect a characteristic sound called the “pericardial rub.” This sound, caused by the inflamed pericardium’s lining, is best heard when you lean forward, hold your breath, and exhale. Depending on the severity of inflammation, crackles in your lungs, suggesting fluid around the lungs or extra fluid in the pericardium, may also be detected.

Pericarditis Tests:-
- Chest X-ray: Checks heart size and lung fluid.
- Electrocardiogram (ECG or EKG): Detects heart rhythm changes. About half of pericarditis cases show specific rhythm alterations, but some may not exhibit any changes. If present, these changes might be temporary.
- Echocardiogram (echo): Assesses heart function and identifies pericardial effusion (fluid around the heart). It also reveals signs of constrictive pericarditis, like a stiff or thickened pericardium affecting heart movement.
- Cardiac MRI: Examines pericardial conditions such as fluid, inflammation, or thickening and checks for heart compression using a contrast agent (gadolinium).
- CT scan: Evaluates calcium deposits, fluid, inflammation, tumors, and conditions around the heart. Iodine dye may enhance information, especially for potential surgery in constrictive pericarditis cases.
- Cardiac catheterization: Provides data on heart filling pressures, confirming constrictive pericarditis diagnosis.
- Blood tests: Rule out a heart attack, assess heart function, test pericardial fluid, and determine pericarditis causes. Elevated sedimentation rate (ESR) and ultra-sensitive C-reactive protein levels indicate inflammation. Additional tests might be needed to assess autoimmune diseases like lupus or rheumatoid arthritis.
Pericarditis treatment:-
In most cases of pericarditis, treatment involves medications specific to the suspected cause. However, if there’s fluid buildup in the pericardium, drainage may be necessary. Surgery might be required for constrictive pericarditis cases.
Treatment for acute pericarditis often involves pain and inflammation medications like ibuprofen or high-dose aspirin. Depending on its cause, antibiotics or antifungal medications might be necessary.
In severe or prolonged cases lasting over two weeks, an anti-inflammatory drug such as colchicine may be prescribed to manage inflammation and prevent future episodes. Prednisone, a steroid, could also be recommended, especially if ibuprofen and colchicine aren’t suitable due to kidney problems.
For high ibuprofen doses, additional medications might be provided to ease stomach issues. Regular check-ups are important when using nonsteroidal anti-inflammatory drugs to monitor kidney and liver function.
Chronic or recurring pericarditis may require long-term NSAID or colchicine use, even during symptom-free periods. Diuretics can help manage fluid retention caused by constrictive pericarditis. Heart rhythm problems may prompt discussions about suitable treatment options.
Further treatment options might involve steroids or medications like azathioprine IV human immunoglobulins, anakinra, or rilonacept for chronic or recurring cases.
If an infection causes pericarditis, specific medicines will target the infection. In cases where cancer is the cause, addressing the cancer itself is the primary treatment.
When fluid collects between the layers of the pericardium, it causes pericardial effusion. Rapid accumulation can lead to cardiac tamponade, a serious compression of the heart affecting its function. This condition is an urgent medical emergency that needs immediate diagnosis and treatment.
This sudden fluid build-up disrupts normal heart function and can cause a drop in blood pressure. Due to the life-threatening nature of cardiac tamponade, swift fluid drainage is crucial.
If pericardial effusion compresses the heart, a procedure called pericardiocentesis may be necessary. Using a catheter guided by echocardiography or a CT scan, healthcare providers drain the excess fluid.
When fluid drainage with a needle isn’t feasible, a minimally invasive surgery called a pericardial window is performed. It involves making a small chest incision to create an opening in the pericardium for fluid drainage.
In constrictive pericarditis cases with scar tissue formation, a surgery called pericardiectomy might be needed to remove part of the pericardium. However, this procedure is generally for individuals with established scar tissue, not those currently experiencing active inflammation and chest pain from pericarditis.
Surgery isn’t commonly used for recurring pericarditis due to challenges in healing post-surgery amid ongoing inflammation. However, if other treatments are ineffective, a doctor may discuss surgery as an option.
